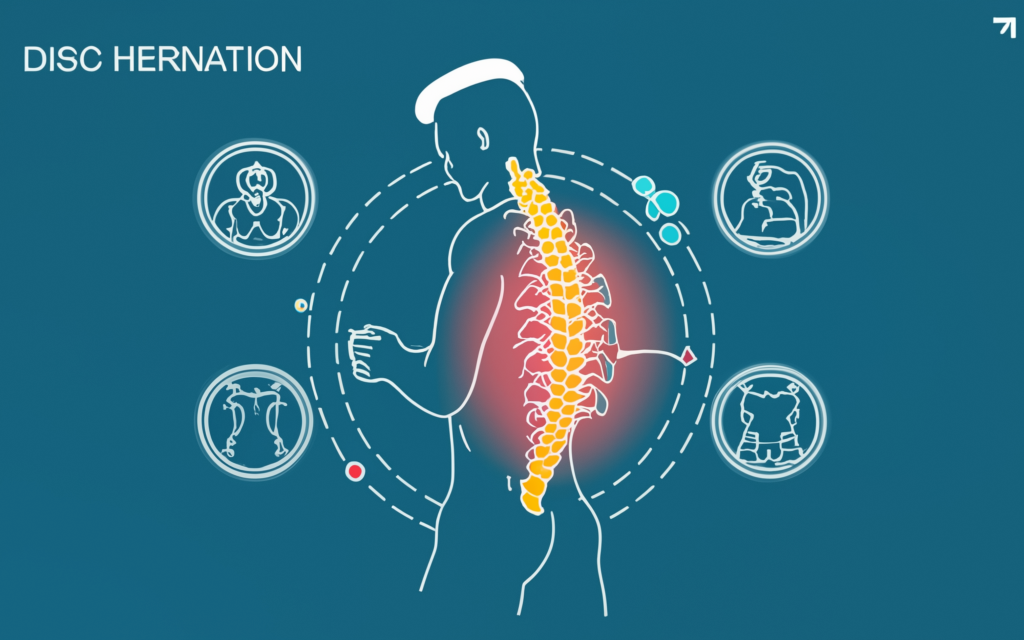
Disc herniation is a condition that influences the spine and can lead to discomfort or restricted movement. Understanding its types, causes, and its effects on the body can help navigate this condition. This article outlines aspects of this condition to provide clarity and insights.
Types of Disc Herniation
Disc herniation can occur in different forms depending on the severity and the location. A contained herniation happens when the disc’s outer layer remains intact but bulges outward due to internal pressure. An extruded herniation occurs when the disc’s inner material pushes through the outer layer, causing potential nerve pressure. If the disc material separates completely and moves away from its original location, it results in a sequestered herniation.
The location along the spine also influences the impact. Cervical herniation involves the neck, often affecting mobility and causing discomfort in the shoulders or arms. A thoracic herniation is less common but can involve pain or nerve issues in the mid-back. Lumbar herniation impacts the lower back and can lead to leg pain or mobility restrictions.
Common Causes of Disc Herniation
Disc herniation can result from various factors, including the natural aging process. Over time, spinal discs lose hydration and elasticity, making them more vulnerable to wear and tear, which increases the risk of herniation. Repetitive strain on the spine is another common cause. Activities like heavy lifting, especially with improper form, can stress the back and lead to disc issues. Prolonged sitting and poor posture further exacerbate this pressure, particularly for those with sedentary lifestyles.
Trauma is another contributing factor, as sudden forces from accidents or falls can strain the discs. Genetic predisposition also plays a role, making some individuals more susceptible to herniation due to inherited weaknesses in their discs. Physical activities involving frequent bending, twisting, or heavy impacts may heighten the risk as well. Balancing physical activity with proper ergonomics and mindful movement can help minimize unnecessary stress on the spine and reduce the likelihood of herniation.
How Disc Herniation Affects the Body
When the inner material of a disc presses on a nerve root, it disrupts communication between the spine and the affected body area. This often results in tingling, numbness, or weakness along the nerve pathway. Localized pain is another common symptom, with the discomfort typically aligning with the site of herniation—for example, neck pain from cervical herniation or lower back pain from lumbar herniation.
Nerve compression often causes pain to radiate into the limbs. Mobility challenges can arise as the spine’s structure is compromised or pain limits movement. Over time, chronic symptoms may lead individuals to alter their posture or movement patterns, which can place additional strain on other parts of the body. Inflammation near the affected area often exacerbates these symptoms by increasing pressure on surrounding structures, further influencing pain and functional limitations.
Not all cases of disc herniation produce noticeable symptoms, but monitoring any changes in comfort, strength, or mobility is necessary. Understanding the physical effects of a herniation allows for a proactive approach to managing the condition, whether through lifestyle adjustments, physical therapy, or other interventions.
Talk with a Specialist Today
If disc herniation has impacted your daily activities or caused discomfort, learning more about your options is helpful. Specialists can evaluate the specific type, cause, and effect of the herniation to recommend suitable solutions. Contact a spine and orthopedic specialist to discuss tailored approaches that meet your needs.