Skin infections are a common medical issue that often result from cuts, scrapes, or puncture wounds. While most skin infections respond well to treatment, certain scenarios can lead to complications. One such complication is skin and bone infections where bacteria spread to deeper layers of the body. This connection between skin and bone holds clinical relevance, particularly for individuals with preexisting health challenges such as diabetes or immunosuppression.
Understanding how skin infections progress and identifying prevention strategies are pivotal in mitigating the risk of deeper infections.
Progression from Skin to Bone Infections
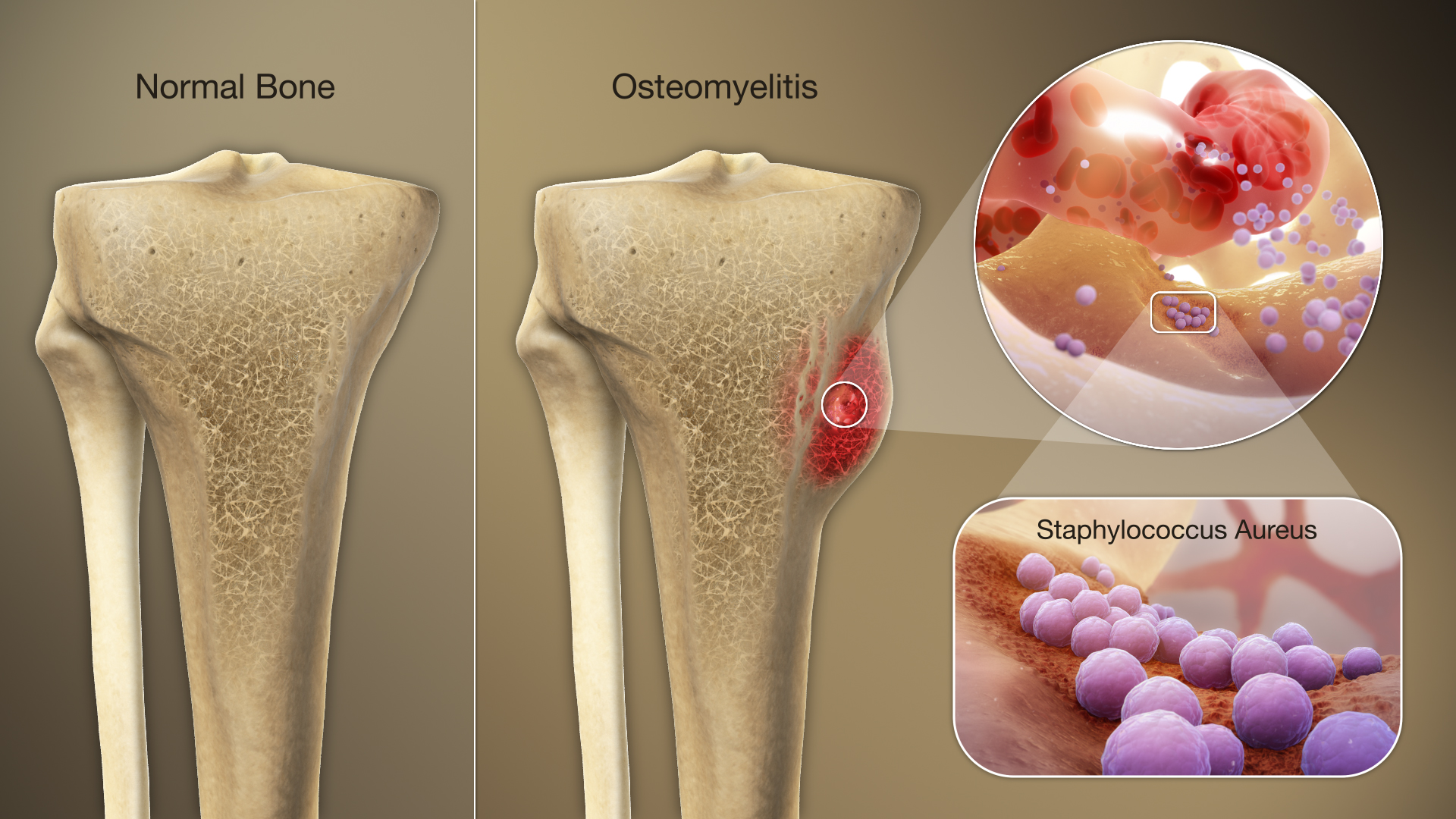
The progression of infection typically follows a pattern, starting from the outermost layers of the skin and traveling inward. When left untreated, bacteria from a skin infection can enter the bloodstream or surrounding tissues, enabling the infection to spread. Once the bacteria reach the bone, conditions such as osteomyelitis (bone infection) can occur.
Common entry points for bacteria include untreated abscesses, ulcers, or prolonged cases of cellulitis. Wounds that fail to heal properly may act as a gateway for pathogens to travel downward, especially in individuals with reduced circulation or compromised immune responses. Skin and bone infections provide a clinical reminder of the interconnectedness of bodily tissues.
Infection Risk Factors to Note
Not everyone with a skin infection is at risk of bone involvement. Specific factors increase susceptibility to the spread of infection. These include:
- Diabetes: Poor blood sugar control often complicates wound healing and increases the likelihood of infection.
- Peripheral Vascular Disease: Limited blood flow to extremities reduces the body’s ability to fight infections.
- Immunosuppression: A weakened immune system, whether due to medications, HIV, or cancer treatments, makes it more difficult for the body to prevent bacterial invasion.
- Deep or Chronic Wounds: Pressure ulcers, particularly in bedridden patients, provide long-lasting entry points for bacteria.
Addressing these underlying conditions early may prevent skin infections from progressing to bone complications.
Signs to Monitor for Skin and Bone Infections
The likelihood of skin infections advancing to bone involvement increases with delays in care. Identifying symptoms early can aid in effective management strategies. Some common symptoms of skin infection include, redness, swelling, warmth in the affected area, pain or tenderness, and fever. If a skin infection spreads to the bone, symptoms may escalate to include chills and reduced mobility in the affected region. Healthcare providers should evaluate any concerning signs promptly, as untreated bone infections may lead to long-term complications, including structural damage or chronic conditions.
Prevention and Early Intervention
Reducing the risk of skin infections spreading to bones begins with enhanced focus on wound care and general health. Specific strategies include:
- Proper Wound Management
- Timely Treatment of Skin Conditions
- Antibiotic Use as Prescribed
Collaboration between patients and healthcare providers can further improve outcomes. Preventative measures tailored to individual health profiles should always remain a priority.
Strategies to Improve Patient Outcomes
The interplay between skin infections and bone infections illustrates how interconnected the body’s systems truly are. When treated early, most skin infections remain manageable. Delayed treatment can result in downstream complications that highlight the need for comprehensive care approaches.