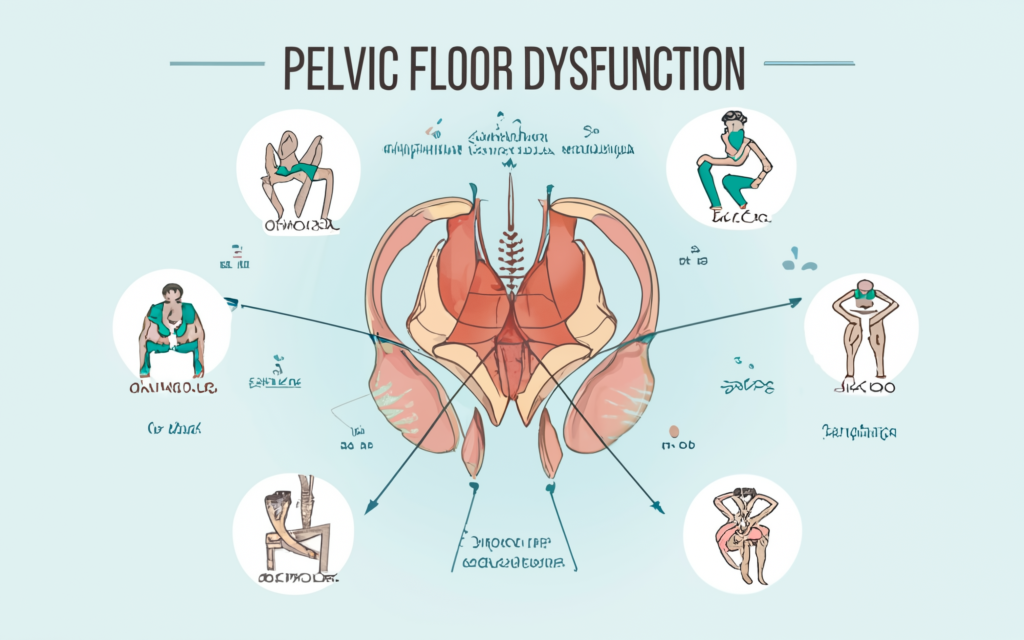
Pelvic floor disfunction can impact individuals of all ages, leading to challenges in daily activities and overall well-being. Symptoms like urinary and bowel issues, along with pelvic pain, can vary greatly, making diagnosis and treatment more complex. Identifying the causes and contributing factors of this condition is essential for managing and improving the quality of life for those affected.
Common Symptoms
Symptoms often include bowel, bladder, or pelvic organ issues. Chronic constipation, urinary or fecal leakage, pelvic pain, pressure in the pelvic area, and frequent, urgent urination are commonly reported. These can greatly impact daily life and overall health.
Common Causes
Pelvic floor disfunction occurs when the muscles and connective tissues supporting pelvic organs, such as the bladder, rectum, and uterus in women, become weakened, overactive, or uncoordinated. Common causes include physical trauma, prolonged stress from pregnancy or childbirth, nerve damage, connective tissue disorders, or chronic strain from constipation or heavy lifting. These factors can compromise the pelvic floor’s ability to function effectively, leading to various symptoms.
Risk Factors
Certain factors increase the risk, including age, which leads to muscle weakness and reduced tissue elasticity. Women are more affected by anatomical differences and childbirth. Obesity adds pressure on the pelvic floor, while heavy lifting or a sedentary lifestyle can also contribute. Previous pelvic surgeries, injuries, or chronic conditions can play a role. Being aware of these risks can aid in early detection and management.
The Role of Aging in
Age weakens muscles and reduces tissue elasticity, increasing risk. Women face added risks from anatomy and childbirth. Obesity, heavy lifting, a sedentary lifestyle, or chronic conditions also contribute. Awareness of these risks helps with early detection and management.
Diagnosis and Treatment Options
Diagnosing this disfunction typically involves a detailed medical history, physical examination, and occasionally specialized tools like imaging tests or biofeedback. Once diagnosed, treatment options vary based on the severity of the condition and underlying causes:
- Physical therapy to strengthen or retrain pelvic floor muscles
- Medications for associated symptoms, such as pain or constipation
- Biofeedback, which uses technology to improve muscle coordination
- Minimally invasive procedures or surgical options for cases requiring structural support
A tailored plan developed in coordination with healthcare providers ensures the best outcomes.
Lifestyle Changes and Prevention Strategies
While some causes of pelvic floor dysfunction cannot be avoided, adopting certain lifestyle changes can help lower risk factors and maintain pelvic health. Regular pelvic floor exercises, like Kegels, can strengthen muscles while managing weight and reducing pressure on the pelvis. A balanced, fiber-rich diet helps prevent chronic constipation, and proper lifting techniques minimize pelvic strain. Staying physically active supports overall muscle health, creating a strong foundation for preventing complications and promoting well-being.
Managing and Treating Pelvic Floor Disfunction
Pelvic floor disfunction can significantly affect an individual’s life, but knowing its causes and addressing symptoms early can offer an opportunity for improvement. Whether exploring preventive steps or considering advanced treatments, prioritizing pelvic health is a step toward enhancing one’s overall quality of life. For guidance tailored to your situation, consult a medical expert or specialist to explore personalized care options that best suit your needs.